an ectopic pregnancy is fatal for the fetus and your pregnancy can't continue. Once an egg implants outside your uterus, you can't move it to your uterus.
Double the uterus, double the babies, double the birthdays: Alabama mom delivers rare twins at UAB
by Hannah EcholsVideography: Mayen Ma, Jeff Myers, Andrea Mabry, Jennifer Alsabrook-Turner, Carson Young
Kelsey Hatcher arrived at the University of Alabama at Birmingham Hospital on Dec. 19 for a scheduled induction for her fourth pregnancy. Many would assume Kelsey’s fourth time giving birth would be a walk in the park, and some may consider her an expert since she had three prior typical, healthy pregnancies.a
However, Kelsey walked into UAB with a pregnancy classified as truly one in a million: She has a rare double uterus and was pregnant with a baby on each side.
After 20 combined hours of labor, she gave birth to two girls, Baby A born Dec. 19 and Baby B born Dec. 20. For Kelsey and her family, this rarity meant double the uterus, double the labor, double the babies and double the birthdays.
“Never in our wildest dreams could we have planned a pregnancy and birth like this; but bringing our two healthy baby girls into this world safely was always the goal, and UAB helped us accomplish that,” Kelsey said. “It seems appropriate that they had two birthdays, though. They both had their own ‘houses,’ and now both have their own unique birth stories.”
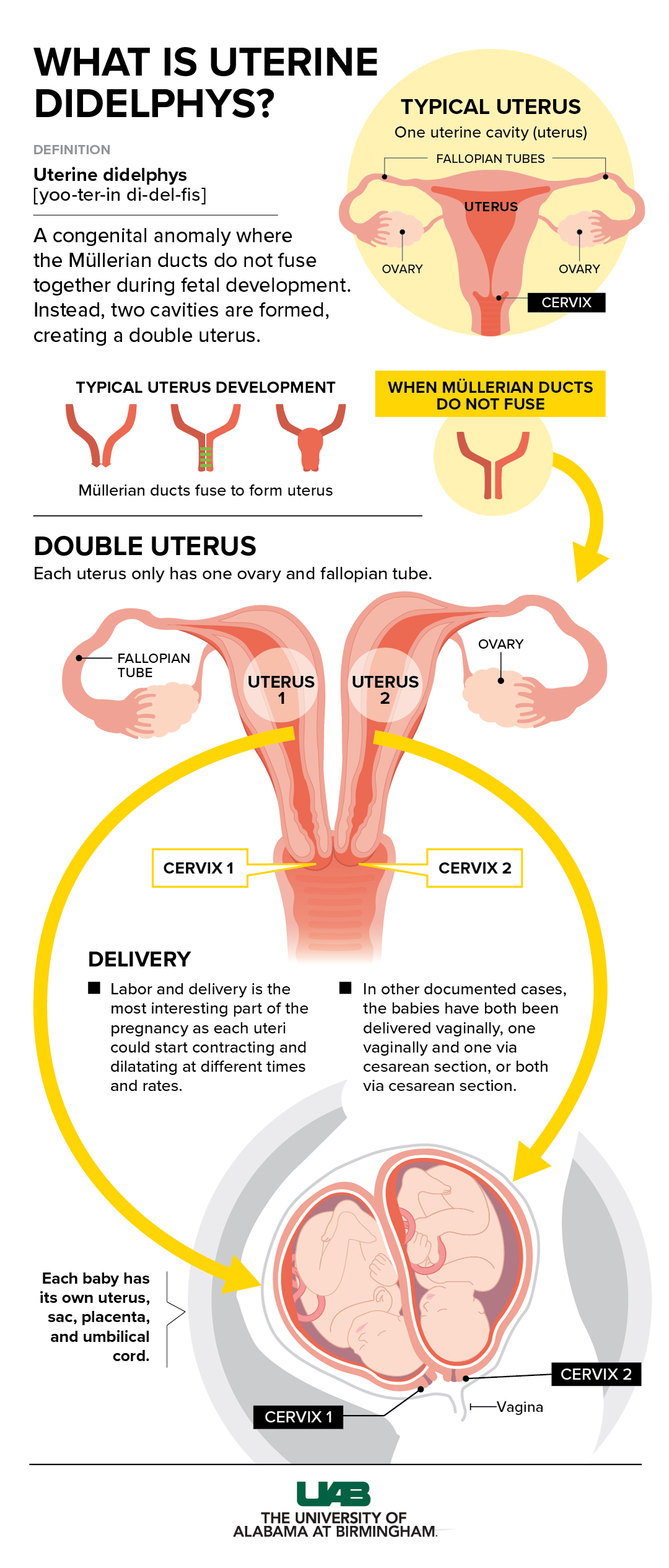
Uterus didelphys is a rare congenital anomaly that occurs in 0.3 percent of women. A dicavitary twin pregnancy occurs when there is a baby in each uterus. Click to enlarge.
Graphic: Jody PotterA one-in-a-million pregnancy
When Kelsey was 17, she was diagnosed with a double uterus — also known as uterus didelphys — a rare congenital anomaly that occurs in 0.3 percent of women. The condition occurs when the Müllerian ducts fail to fuse together and subsequently form two uterine cavities, often referred to as “horns.” Each uterus has one fallopian tube and one ovary. In Kelsey’s case, she also has two cervices.
A few weeks into her fourth pregnancy, Kelsey noticed some bleeding. Since women with a double uterus are at a higher risk of miscarriage, she made an appointment for her first ultrasound. After the UAB ultrasound showed the baby was doing well, Kelsey asked her to check her second uterus for good measure.
“As soon as she moved the wand to the other uterus, I gasped,” Kelsey recalled. “Sure enough, there was another baby. We just could not believe it.”
Kelsey’s obstetrician, Shweta Patel, M.D., assistant professor in the UAB Department of Obstetrics and Gynecology, was in disbelief of the discovery until she was able to look at the scans herself. While it is not as uncommon for women with a double uterus to have a pregnancy with one baby in one uterus, as Kelsey had carried three times before, having a baby in both — also known as a dicavitary pregnancy — is an estimated one-in-a-million chance.
“I had already taken care of Kelsey through her third pregnancy and knew she had a double uterus, but that was only one baby — two babies in two uteri were a true medical surprise,” Patel said. “I knew I would need additional expertise. Luckily, I was able to reach out to my UAB maternal-fetal medicine colleagues who specialize in high-risk obstetrics cases and unique pregnancies.”
Over the next nine months, Kelsey rotated between her obstetrics and maternal-fetal medicine team for routine checkups and ultrasounds. Other than a few additional appointments, her pregnancy was routine.
“In a typical twin pregnancy, the twins share one womb, which can limit the amount of space each has, making preterm or early birth a high possibility,” said Richard O. Davis, M.D., professor in the UAB Division of Maternal-Fetal Medicine who co-managed Kelsey’s pregnancy. “With Kelsey’s babies, they each had their own womb, sac, placenta and umbilical cord, allowing them extra space to grow and develop.”
While ongoing monitoring gave Kelsey’s obstetrics teams peace of mind during pregnancy, forecasting for her imminent delivery and all the possibilities on the table was something that UAB experts had never had to plan for before.
Planning for the unknown
Due to the rareness of dicavitary twins, Patel and Davis had only a handful of case reports to study and use to guide a plan for delivery. In some cases, both babies were born vaginally; in others, the cervices would dilate only to a certain point, thus resulting in a double cesarian section. There were also cases where one uterus went into spontaneous labor and the other did not.
The team knew there were three potential delivery scenarios:
- Both babies delivered vaginally
- One baby delivered vaginally, the other delivered via c-section
- Both babies delivered via c-section
“While c-sections may be a more controlled delivery option for high-risk cases like this one, we did not want to jump to the third plan immediately, knowing Kelsey’s history of successful vaginal births from both uteri,” Patel said. “We also listened to Kelsey’s wishes. She wanted to aim to have the same birth experience for the girls as her other children, if safe and possible.”
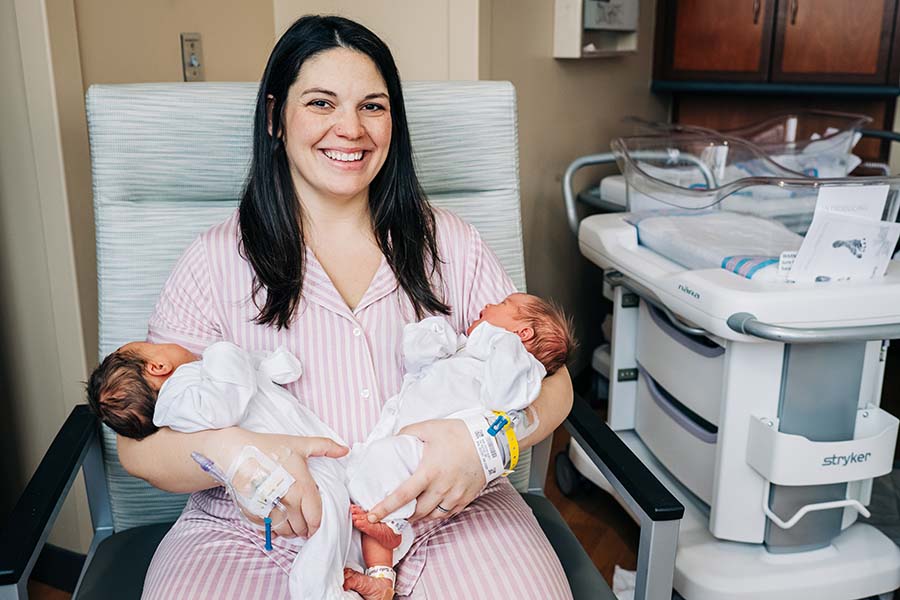
 Left: Baby A, named Roxi, was delivered vaginally on Dec. 19 at 7:45 p.m. weighing 7 pounds 7 ounces. Right: Baby B, named Rebel, was delivered via c-section on Dec. 20 at 6:10 a.m. weighing 7 pounds 3.5 ounces.
Left: Baby A, named Roxi, was delivered vaginally on Dec. 19 at 7:45 p.m. weighing 7 pounds 7 ounces. Right: Baby B, named Rebel, was delivered via c-section on Dec. 20 at 6:10 a.m. weighing 7 pounds 3.5 ounces.
Photography: Andrea MabryDouble labor, double birthdays
The ideal scenario would have been for Kelsey to go into labor on her own. But since spontaneous labor did not occur, she was induced at 39 weeks. When Kelsey arrived at the UAB Women and Infants Center early in the morning of Dec. 19, she was dilated 4 cm on her right cervix and 3 cm on her left.
The team began the induction process and waited to see if one baby would progress further than the other. Since she had two uteri, she required twice the monitoring and charting, and was assigned two labor and delivery nurses to monitor each uterus and baby.
“As my contractions began, they were not consistently together but were within a few seconds of each other,” Kelsey said. “I felt each side contracting in different areas as well. I felt one consistent with the monitor that started on the left side and moved to the right.”
Her right uterus — which had already had two pregnancies — began progressing further than the left, and the baby’s head was lower. The team decided to focus on the baby on the right and moved ahead with breaking her water on that side. A few hours later, Baby A, named Roxi, was delivered vaginally at 7:45 p.m. weighing 7 pounds 7 ounces.
“There was a cheer from everyone in the room when the first baby was delivered, but there was another baby left,” Patel said. “Kelsey was essentially laboring in the left uterus while simultaneously undergoing the postpartum process in the right. She was having contractions with Baby B while breastfeeding Baby A.”
There was not a set blueprint on how to anticipate the birth of the second baby, so the team listened to Kelsey and Baby B for the best course of action. They continued with an induction on the left side, but Baby B was not descending as anticipated for another vaginal delivery. A little over 10 hours after her sister was born, Baby B, named Rebel, was delivered via c-section on Dec. 20 at 6:10 a.m. weighing 7 pounds 3.5 ounces.
The nursing team arranged for Baby A’s bassinet to be in a safe area of the operating room for Baby B’s delivery, allowing the siblings to finally meet.
“After such a long and crazy journey, it meant the world to see both of my girls together for the first time,” Kelsey said.
 Kelsey holds Roxi while her husband, Caleb, holds Rebel. Photography: Andrea MabryTwins ... or not?
Kelsey holds Roxi while her husband, Caleb, holds Rebel. Photography: Andrea MabryTwins ... or not?
Prior to Kelsey’s case, neither Patel nor Davis, who have close to a combined 60 years of experience, had delivered dicavitary twins. They relied on each other and the rest of the UAB women’s health team to combine evidence-based data with their obstetrical expertise to go into the unknown and come out with two healthy babies and a healthy mom.
“It goes to show that the field of obstetrics is always changing and unpredictable, and you don’t always have clear-cut answers,” Patel said. “It takes a team of experts from obstetricians to amazing nurses and a skilled anesthesia team to take care of such a rare pregnancy. I am grateful that Kelsey was at UAB, where we could provide her with that interdisciplinary care.”
With two wombs and two birthdays, the question remains, are the babies twins? Technically, yes and no.
A typical twin pregnancy is defined by two babies in one uterus during the same pregnancy.
While Kelsey had one baby in each uterus, two eggs were released that were fertilized during the same ovulation cycle.
“I think it is safe to call the girls fraternal twins,” Davis said. “At the end of the day, it was two babies in one belly at the same time. They just had different apartments.”






No comments:
Post a Comment